Mini-Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Dyslipidemias in Children and Adolescents
*Corresponding author:Tania Leme da Rocha Martinez, A Beneficência Portuguesa de São Paulo, São Paulo, Brazil
Received:March 29, 2023;Published:April 21, 2023
DOI: 10.34297/AJBSR.2023.18.002495
Abstract
The prevalence of dyslipidemia in children and adolescents varies worldwide between 2.9 and 33%, adopted as a criterion the level of total cholesterol higher than 200 mg/dL. In Brazil, the prevalence is between 28 and 40% of children and adolescents, when the criterion adopted is serum total cholesterol greater than 170 mg/dL. After 10 years of age, it is already possible to perform tests to trace the lipid profile, because it is easier to keep the child fasting and the rates presented are close to those that will be maintained during adolescence and adulthood. In summary, every child should be screened for dyslipidemias at 10 years of age. For younger children, between 2 and 10 years of age, screening is indicated if: parents, grandparents, siblings and first cousins have dyslipidemia, mainly severe or manifestation of premature atherosclerosis (total cholesterol 300 or triglycerides 400 mg/dL); clinical dyslipidemia (positive history of acute pancreatitis, eruptive xanthomas, eyelid corneal arch, ankle xanthomas, dorsal face of the hands and knees); have other risk factors; there is exposure to other diseases, such as hypothyroidism, nephrotic syndrome, systemic lupus erythematosus, diabetes mellitus, immunodeficiency, etc.; contraceptives, immunosuppressants, corticosteroids, antiretrovirals and other drugs that may induce cholesterol elevation and unknown family history are used.
Keywords: Cholesterol, Triglycerides, Children, Adolescents, Coronary Heart Disease Risk
Abbreviations:ACD: Atherosclerotic Disease; HDL-c: High Density Lipoprotein Cholesterol; LDL-c: Low Density Lipoprotein Cholesterol; NCEP: National Cholesterol Education Program; TC: Total Cholesterol; TG: Triglycerides
Introduction
There is much evidence that the atherosclerotic process
begins to develop in childhood [1-6]. Autopsy studies in children
demonstrate a strong positive association between pre-death Low
Density Lipoprotein Cholesterol (LDL-c) levels and the presence
of fatty stretch marks at the aortic level [2]. Although there are
controversies, studies focused on the segment of cholesterol levels
from childhood to adulthood indicate that children, located at the
upper end of the cholesterol distribution curve, have a 40 to 50%
chance of remaining hypercholesterolemic 15 to 20 years later [7-
8]. This percentage, in addition to genetic influences, is directly
linked to the lifestyle adopted by the child and his family [9]. In
addition, in countries where morbidity and mortality rates due
to cardiovascular disease are high, both adults and children have
cholesterol levels higher than those recommended by the consensus
on dyslipidemia [10]. According to the National Cholesterol
Education Program (NCEP) [10] and the latest Brazilian Consensus
on Hyperdyslipidemia [11], the systematic determination of the
lipid profile in childhood is not recommended, and should be
performed only in special situations:
1. Grandparents, parents, siblings, uncles and first cousins
with presenting atherosclerotic disease (ACD) (ACD and/or
cerebrovascular and/or peripheral disease) before the age of 55 for
males, and 65 years for females.
2. Close relatives with total cholesterol (TC) > 300 mg/dL or
triglycerides (TG) ≥ 400 mg/dL.
3. Presence of acute pancreatitis, xanthomatosis, obesity, or
other risk factors for ACD.
At birth, the measurements of TC, LDL-c and High-Density Lipoprotein Cholesterol (HDL-c) are 70, 30 and 35 mg/dL respectively. With the introduction of a higher fat content in the diet, these values tend to increase rapidly. It is recommended to evaluate the lipid profile from the second year of life, because it is around this age that the cholesterol level that should be maintained throughout the first decade is reached [12]. Puberty, due to fluctuations in lipid levels, due to hormonal changes, may offer some degree of difficulty in evaluating the results of lipid profile dosage [13]. It is extremely important that the laboratory results obtained, especially when abnormal, are repeated. A diagnosis of dyslipidemia can generate a high degree of anxiety. Studies have revealed that a positive laboratory report for dyslipidemia has long-term psychological effects, both in children and in their families, even when it is later reported to be a false positive case [14,15].
We remind you that the isolated dosage of TC, as a way of screening dyslipidemic children, is subject to failures. Children with elevated LDL-c level and decreased HDL-c may have normal TC levels and go unnoticed at screening. In addition, children with elevated TG levels would not be screened. We recall that the most common changes in the lipid profile of obese children are: decrease in HDL-c and increase in TG.
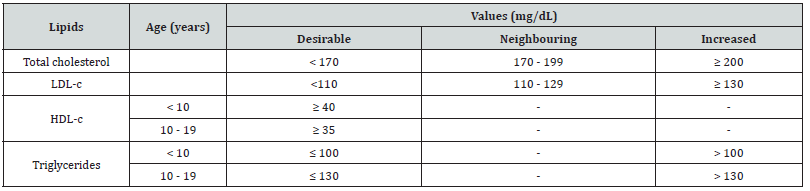
(Table 1) illustrates the reference values for the lipid profile for children and adolescents accepted by the most recent Brazilian Consensus on Hyperdyslipidemia, according to Kwiterovich’s recommendations.
Treatment Itself
Once the normal levels and consequently the goals to be achieved are known, we will begin to address the stages of treatment.
Lifestyle Changes
Diet
Diet is the cornerstone of the treatment of dyslipidemias
in childhood. We must remember that nutritional errors are
responsible for most of the changes in the lipid profile found in
children and adolescents [11,16,17]. The introduction of nutritional
modifications in childhood is related to greater adherence, since
eating habits and patterns are in formation[10,16]. However,
during the elaboration of the diet and the orientation given to the
family, some care should be taken.
a. Nutritional guidance should always be individualized.
The calculation of daily caloric intake aims to keep the child at
an adequate weight and ensure their growth and development.
Extremely restrictive diets have deleterious effects [18].
b. Nutritional adequacy must be achieved through a
wide variety of foods. Food monotony can lead to unwanted
transgressions.
c. The guidelines given to the child should be incorporated
by the family. This measure, in addition to being vital for adherence
to treatment, has a positive psychological effect: the child does not
see himself sick, but rather acquiring new eating habits like the
other members of his family.
d. When prescribing the diet, the professional should prove
himself safe. Some parents, alarmed by the report of dyslipidemia,
tend to exceed the guidelines given [19].
According to the NCEP, dietary therapy is divided into two phases [10]. The phase 1 diet is prescribed when LDL-c levels are 130 mg/dL. If lipid levels have not normalized, after adequate adherence to the guidelines given for at least 3 months, a more restricted diet is prescribed.
Physical Activity
When performed on a regular basis, it promotes the reduction of TC and an increase in HDL-c levels. In addition, it contributes to the acquisition/maintenance of ideal weight [13].
Other Lifestyle Modifications
Smoking should be discouraged. Since its effect is dose dependent, it is clear that the magnitude of the risk it provides is exacerbated when the habit of smoking begins in childhood. In the Pathobiological Determinants of Atherosclerosis in Youth Program (PDAY) it was demonstrated that smoking (assessed through the level of thiocyanate in serum) is able to promote atherogenic process in adolescents up to 15 years old [20]. Many authors consider obesity to be an independent risk for ACD [21]. This condition is associated with lipid changes, which usually normalize with weight loss. In addition, the presence of obesity in childhood has a predictive value for its maintenance in adulthood [22], so it should be treated as early and as possible.
Contraceptive use is associated with changes in lipid profile. As the use of this type of medication is a reality among our adolescents, guidance should be given regarding the choice of the pill. Ideally, one should opt for one that has low estrogen and progestogen dosages, and that the progestogen in question does not contain androgenic activity.
Drug Therapy
When lifestyle modifications are not sufficient to reverse dyslipidemia, then the use of lipid-lowering drugs is associated with the therapeutic plan. According to the recommendations of the NCEP, it is only recommended in children over 10 years of age and, in general, should only be introduced if, after a period of 6 months to 1 year of adherence to lifestyle modifications, there is no normalization of the lipid profile [10]. That is, when after the period described, cholesterol levels remain ≥ 190 mg/dL or > 160 mg/dL in children with a family history of premature cardiovascular disease and in those with two or more risk factors for cardiovascular disease.
Bile acid scavengers (cholestyramine and colestipol) make up the most accepted group of drugs for pediatric use and the only ones approved by the NCEP. The light questran (cholestyramine) is the only representative of this group of commercially available drugs in Brazil. These medications are not absorbed and exert their action at the intestinal level. By binding to bile acids in the gut, they reduce their enterohepatic circulation, leading to an increase in LDL-c receptors in the liver [23]. Side effects are less prominent in children than in adults. Intestinal constipation, the most common of them, can be minimized by introducing fiber into the diet. Because they are related to the decrease in the absorption of fatsoluble vitamins (A, D, E) and folate, in addition to concomitantly administered medications, it is suggested that an interval of at least 2 and a half hours be maintained between the use of bile acid sequestrants and meals/use of other drugs [23]. In some cases, folic acid supplementation 5 mg/day may be necessary.
Dosage calculations are based on LDL-c levels and not on children’s weight. The suggested starting dose is 4 g/day. The usual maximum dose is 16 g/day [23]. Nicotinic acid represents another alternative for the treatment of hypercholesterolemic children. However, it should only be prescribed by specialists [10]. In general, its use is made in association with the sequestrant of bile acid, when the same, alone, is not able to reduce LDL-c levels properly. The side effects arising from its use require prior clarification to the patient and his family. The vast majority of patients present with skin reactions (flushing and heat) after its administration. Previous use of aspirin 30 minutes before can minimize these effects [24-26] and its administration should precede that of nicotinic acid about 10 days.
Omega-3 fatty acid should be seen more as a dietary supplement than as a drug itself. Its use is related to the reduction of Very Low- Density Lipoprotein Cholesterol (VLDL-c) and TG levels. However, its action on LDL and HDL-c is controversial [27]. Medications, such as Vastatins, due to the small current experience, can be used in cases of severe familial hypercholesterolemia (TC > 300 mg/dL and/or manifest ACD, in which the use of resins was unsatisfactory) [10].
Conclusion
The evaluation and treatment of dyslipidemias in childhood and adolescence should not be neglected. Early intervention is able to prevent future atherosclerotic manifestations. In addition to the individual approach to dyslipidemia, discussed throughout this chapter, we would like to focus on the importance of the population approach. The adoption of healthy lifestyle habits such as a balanced diet, without excess saturated fat, regular physical activity, maintenance of ideal weight and combating smoking, should be adopted by the general population. Obviously, this type of approach requires the support of groups and entities that can collaborate with the implementation of the proposed measures: health professionals, schools, government agencies, food industries and the media.
Acknowledgments
None.
Conflicts of interest
No conflict of interest.
References
- Kaprio J, Norio R, Pesonen E, Sarna S (1993) Intimal thickening of the coronary arteries in infants in relation to family history of coronary artery disease. Circulation 87(6): 1960-1968.
- Newman WP 3rd, Wattigney W, Berenson GS (1991) Autopsy studies in United States children and adolescents. Relationship of risk factors to atherosclerotic lesions. Ann N Y Acad Sci 623: 16-25.
- Holman RL, McGill HC Jr, Strong JP, Geer JC (1958) The natural history of atherosclerosis: the early aortic lesions as seen in New Orleans in the middle of the of the 20th century. Am J Pathol 34(2): 209-235.
- Stary HC (1989) Evolution and progression of atherosclerotic lesions in coronary arteries of children and young adults. Arteriosclerosis 9(1 Suppl): I19-I32.
- Stary HC (1990) The sequence of cell and matrix changes in atherosclerotic lesions of coronary arteries in the first forty years of life. Eur Heart J 11 Suppl E: 3-19.
- Strong JP (1986) Landmark perspective: Coronary atherosclerosis in soldiers. A clue to the natural history of atherosclerosis in the young. JAMA 256(20): 2863-2866.
- Webber LS, Srinivasan SR, Wattigney WA, Berenson GS (1991) Tracking of serum lipids and lipoproteins from childhood to adulthood. The Bogalusa Heart Study. Am J Epidemiol 133(9): 884-899.
- Stuhldreher WL, Orchard TJ, Donahue RP, Kuller LH, Gloninger MF, et al. (1991) Cholesterol screening in childhood: sixteen-year Beaver County Lipid Study experience. J Pediatr 119(4): 551-556.
- Kwiterovich PO Jr (1986) Biochemical, clinical, epidemiologic, genetic, and pathologic data in the pediatric age group relevant to the cholesterol hypothesis. Pediatrics 78(2): 349-362.
- (1992) National Cholesterol Education Program (NCEP): highlights of the report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics 89(3): 495-501.
- Faludi AA, Izar MCO, Saraiva JFK, Ana Paula Marte Chacra, Henrique Tria Bianco, et al. (2017) Atualização da Diretriz Brasileira de Dislipidemias e Prevenção da Aterosclerose - 2017. Arq Bras Cardiol 109(2Supl.1): 1-76.
- Kwiterovich PO, Levy RI, Fredrickson DS (1973) Neonatal diagnosis of familial type-II hyperlipoproteinaemia. Lancet 1(7795): 118-121.
- Strong WB, Deckelbaum RJ, Gidding SS, R E Kavey, R Washington, et al. (1992) Integrated cardiovascular health promotion in childhood. A statement for health professionals from the Subcommittee on Atherosclerosis and Hypertension in Childhood of the Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 85(4): 1638-1650.
- Feldman W (1990) Routine cholesterol surveillance in childhood. Pediatrics 86(1): 150-151.
- Cayler GG, Lynn DB, Stein EM (1973) Effect of cardiac nondisease on intellectual and perceptual motor development. Br Heart J 35(5): 543-547.
- Widhalm K (1987) Paediatric guidelines for lipid reduction. Eur Heart J 8(suppl E): 65-70.
- (1995) Efficacy and safety of lowering dietary intake of fat and cholesterol in children with elevated low-density lipoprotein cholesterol. The Dietary Intervention Study in Children (DISC). The Writing Group for the DISC Collaborative Research Group. JAMA 273(18): 1429-1435.
- Cetta F, Driscoll DJ, Lucas AR, R L Urevig, D M Huse, et al. (1994) Growth patterns of hyperlipidemic children enrolled in a preventive cardiovascular health clinic. Clin Pediatr (Phila) 33(10): 588-592.
- Mietus Snyder M, Baker AL, Neufeld EJ, C Roberts, S Dermarkarian, et al. (1993) Effects of nutritional counseling on lipoprotein levels in a pediatric lipid clinic. Am J Dis Child 147(4): 378-381.
- (1990) Relationship of atherosclerosis in young men to serum lipoprotein cholesterol concentrations and smoking. A preliminary report from the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. JAMA 264(23): 3018-3024.
- Carruthers SG (1993) Cardiovascular risk factors in perspective. Can Fam Physician 39: 309-314.
- D S Freedman, C L Shear, G L Burke, S R Srinivasan, L S Webber, D W Harsha, et al. (1987) Persistence of juvenile-onset obesity over eight years: the Bogalusa Heart Study. Am J Public Health 77(5): 588-592.
- Farah JR, Kwiterovich PO Jr, Neill CA (1977) Dose-effect relation of cholestryamine in children and young adults with familial hypercholesterolaemia. Lancet 1(8002): 59-63.
- Grundy SM, Mok HY, Zech L, Berman M (1981) Influence of nicotinic acid on metabolism of cholesterol and triglycerides in man. J Lipid Res 22(1): 24-36.
- Luria MH (1988) Effect of low-dose niacin on high-density lipoprotein cholesterol and total cholesterol/high-density lipoprotein cholesterol ratio. Arch Intern Med 148(11): 2493-2495.
- R H Knopp, J Ginsberg, J J Albers, C Hoff, J T Ogilvie, G R Warnick, et al. (1985) Contrasting effects of unmodified and time-release forms of niacin on lipoproteins in hyperlipidemic subjects: clues to mechanism of action of niacin. Metabolism 34(7): 642-650.
- Demke DM, Peters GR, Linet OI, Metzler CM, Klott KA (1988) Effects of a fish oil concentrate in patients with hypercholesterolemia. Atherosclerosis 70(1-2): 73-80.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.